RED FLAGS IN SPINE
Red flag is defined as something that gives a warning of trouble. In spine there are some patient’s symptoms and clinical features which behave as red flags for the underlying spinal disease. These red flags help the surgeon in diagnosis and treatment of various pathological conditions of spine.
Early diagnosis of spine pathology with the help of red flags results in early and better treatment of the disease condition. It is better if everyone knows about these red flags. People who have idea about these red flags can have self assessment and seek medical opinion at the earliest. If red flags are present in any individual then, a suspicion of under lying serious spinal pathology should caution treating surgeon for appropriate clinical evaluation and investigations to confirm the same.
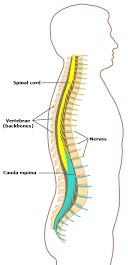
Various red flag signs and symptoms are routinely used in the assessment of low back pain, neck pain or to identify spinal cord emergencies. These spinal conditions can be divided into following categories:
- Spinal fractures
- Malignancy
- Infections
- Spinal cord compression
- Cauda equine syndrome
The red flags used most commonly for identifying spinal cord compression, irrespective of the aetiology are:
- Profound motor or sensory weakness in the lower extremities
- Bowel or bladder dysfunction
- Saddle distribution sensory disturbance.
Sudden loss of bowel or bladder control can result from the pinching of the nerves to the bladder and bowel or compression of spinal cord within the spinal canal. This can also be associated with loss of sensation at the buttocks, inner part of thighs and legs or weakness of the legs. These symptoms due to pinching of the nerves in the lumbar spine, is known as cauda equina syndrome. This is an emergency spinal condition requiring immediate evaluation of your spine by a spine surgeon.

The red flags which are used as a warning of danger and indicators of serious underlying spinal pathology are as follows: (Chronic low back pain.BMJ 2003; 326 doi: https://doi.org/10.1136/ bmj.326.7388.535)
- Thoracic pain
- Fever
- unexplained weight loss
- Bladder or bowel dysfunction
- History of carcinoma
- Ill health or presence of other medical illness
- Progressive neurological deficit
- Disturbed gait
- Saddle anaesthesia
- Age of onset <20 years or >55 years
Arm or leg weakness is a sign of nerve injury and should be assessed by a spine and nerve specialist at the earliest after onset. The treatment includes medications and therapy, spinal or other nerve injections, or timely surgical intervention.
Severe head, neck, or back pain, especially when associated with following red flag signs, requires immediate assessment by a spine physician:
- Trauma (fall from height, road traffic accident, assault, weight lifting)
- Fever, chills or sweats
- Neurological signs such as
- Weakness or clumsiness of hands / legs
- Numbness or tingling in hands and legs
- Loss of bowel or bladder control
- Stumbling or falling
- Pain at rest
- Pain at night
- Rapid fatigue
- Prolonged use of steroids
- Bending towards one side
- Tuft of hairs on lower back at birth
- Symptoms of brain dysfunction such as
- Confusion
- Speech problems
- Visual disturbances


Either individual red flags or combinations of red flags are associated with an increased probability of underlying serious spinal pathology, e.g., recent trauma and an age of >50 years were associated with vertebral fracture2.
As we read above that red flag signs give a clue about the possibility of underlying spinal pathology but, many a times it happens that many people with underlying spinal pathology does not show any red flags. 64% of patients with spinal malignancy had no associated red flags2. So, one should not wait for red flags to show before seeing a spine surgeon or totally depend on them but act according to the real health condition of the patient.
References
1. Chronic low back pain.BMJ 2003; 326 doi: https://doi.org/10.1136/ bmj.326.7388.535
Ajay P, William G, Michael G, Scott B. Red Flags for Low Back Pain Are Not Always Really Red: A Prospective Evaluation of the Clinical Utility of Commonly Used Screening Questions for Low Back Pain. The Journal of Bone and Joint Surgery: March 7, 2018 – Volume 100 – Issue 5 – p 368-374 doi: 10.2106/JBJS.17.00134