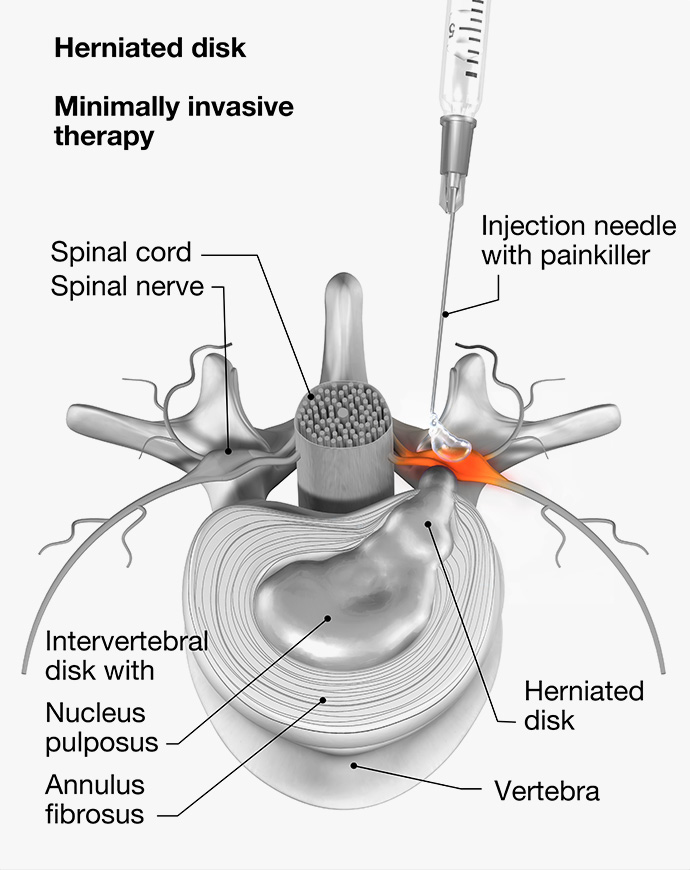
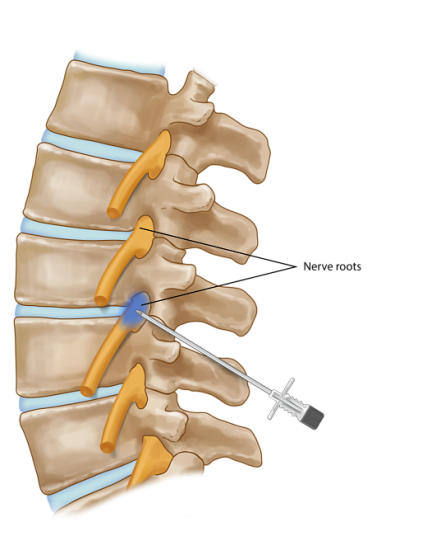
The most common indications for nerve root block include radicular pain caused by herniated discs, spinal stenosis, and degenerative disc disease. The procedure is also used to treat pain caused by nerve compression in the cervical, thoracic, and lumbar regions of the spine.
The procedure is typically performed under fluoroscopic guidance, which allows the physician to see the exact location of the needle and to ensure that the medication is being injected into the correct area. A small amount of local anesthetic is injected to numb the area, followed by the injection of a corticosteroid. The corticosteroid works to reduce inflammation and swelling around the affected nerve, which can help to alleviate pain and improve function.
The procedure is generally considered to be safe, with few complications reported. However, as with any medical procedure, there are potential risks and side effects, including pain at the injection site, infection, bleeding, and nerve damage.
The effectiveness of nerve root block as a treatment option for radicular pain has been widely studied. A systematic review and meta-analysis published in the Journal of Orthopaedic Surgery and Research found that nerve root block is an effective treatment option for lumbar radicular pain caused by herniated discs, with a significant reduction in pain reported by patients. Another study published in the Journal of Neurosurgery: Spine found that nerve root block is an effective treatment option for cervical radicular pain caused by herniated discs and spinal stenosis.
In conclusion, nerve root block is a common procedure used to diagnose and treat pain caused by nerve compression in the spine. The procedure involves the injection of a local anesthetic and a corticosteroid into the area around the affected nerve root. The procedure is considered to be safe, with few complications reported and is effective treatment option for radicular pain caused by herniated discs, spinal stenosis, and degenerative disc disease.